California law requires all food handlers to have certification in handling major food allergens and preventing cross-contamination.
AB 1532 (The Natalie Giorgi Sunshine Act) – amends Section 113947 of the California Health and Safety Code – to require all food handlers to have a simple certification in safe food handling practices for major food allergens.
AB 1532 also added “Organized Camps” to the definition of “Food Facility” for the basis of requiring training for individuals who handle food at camps. This is due to Natalie Giorgi passing away at age 13 due to a severe allergic reaction to undeclared peanut in a treat while at a summer camp in Sacramento.
Food service operations can greatly reduce the risk for allergic reactions among patrons by providing food allergy training for all food-handling personnel, list ingredients for patrons on all menu items, and by dedicating equipment and areas specifically for preparing allergen-free food.
California Food Allergy Law (Cal Code)
Section 113947 of the California Health and Safety Code:
(a) The person in charge and all food employees shall have adequate knowledge of, and shall be properly trained in, food safety as it relates to their assigned duties.
(b) The person in charge shall comply with both of the following:
(1) Have adequate knowledge of major food allergens, foods identified as major food allergens, and the symptoms that a major food allergen could cause in a sensitive individual who has an allergic reaction.
(2) Educate the employees at the food facility regarding the information described in paragraph (1), which the person in charge may elect to accomplish by, among other methods, using a poster or job aid to which the employee can refer.
(c) For purposes of this section, “person in charge” means a designated person who has knowledge of safe food handling practices and the major food allergens as they relate to the specific food preparation activities that occur at the food facility.
Food Allergy Statistics
According to Food Allergy Research and Education (FARE), about 32 million people in the U.S. have food allergies (and 5.6 million of those are children under age 18).
- Learn the best practices for serving a food allergic customer including: the role of management, how to properly prepare an allergen safe meal, and the front of the house and back of the house responsibilities.
- Reg Price: $15.00
- Enter Code "train10off" at Checkout
Likewise, the Centers for Disease Control & Prevention (CDC) reports that the prevalence of food allergy in children increased by 50 percent between 1997 and 2011. And between 1997 and 2008, the prevalence of peanut or tree nut allergy appears to have more than tripled in U.S. children.
What is a Food Allergy?
- A food allergy is a medical condition in which exposure to a food triggers a harmful immune response. The immune response, called an allergic reaction, occurs because the immune system attacks proteins in the food that are normally harmless. The proteins that trigger the reaction are called allergens.
- The symptoms of an allergic reaction to food can range from mild (itchy mouth, a few hives) to severe (throat tightening, difficulty breathing).
- Anaphylaxis is a serious allergic reaction that is sudden in onset and can cause death.
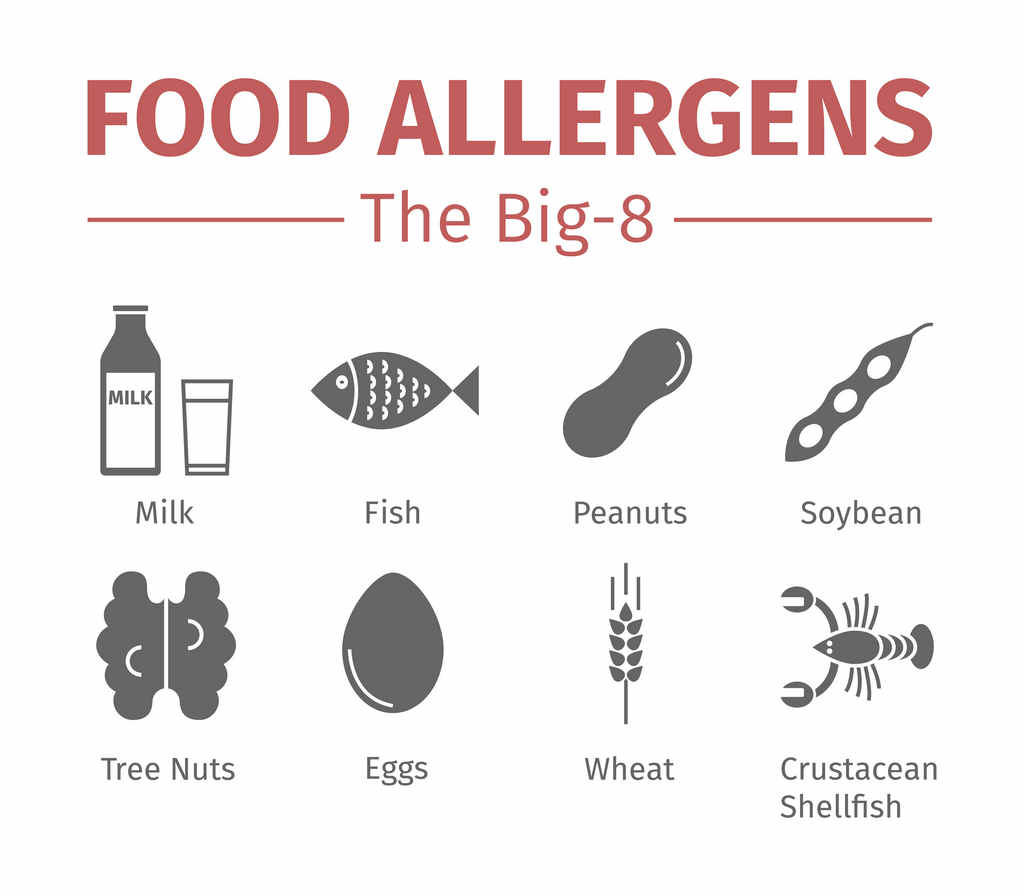
What are the Major Food Allergens?
While more than 160 foods can cause allergic reactions in people with food allergies, the law identifies the eight most common allergenic foods. These foods account for 90 percent of food allergic reactions, and are the food sources from which many other ingredients are derived.
The eight foods identified by the law as food allergens are:
- Milk
- Eggs
- Fish (e.g., bass, flounder, cod)
- Crustacean shellfish (e.g., crab, lobster, shrimp)
- Tree nuts (e.g., almonds, walnuts, pecans)
- Peanuts
- Wheat
- Soybeans
These eight foods, and any ingredient that contains protein derived from one or more of them, are designated as “major food allergens” by the Food Allergen Labeling and Consumer Protection Act (FALCPA).
Food Allergy Labeling and Consumer Protection Act (FALCPA)
In 2004, Congress passed the Food Allergen Labeling and Consumer Protection Act (FALCPA). This law requires food labels to list common allergens in the ingredients.
This law does not apply to prepared food — only packaged items. As a result, many states have enacted allergen laws that specifically apply to restaurants.
FDA Video: Food Allergies – Reducing the Risks
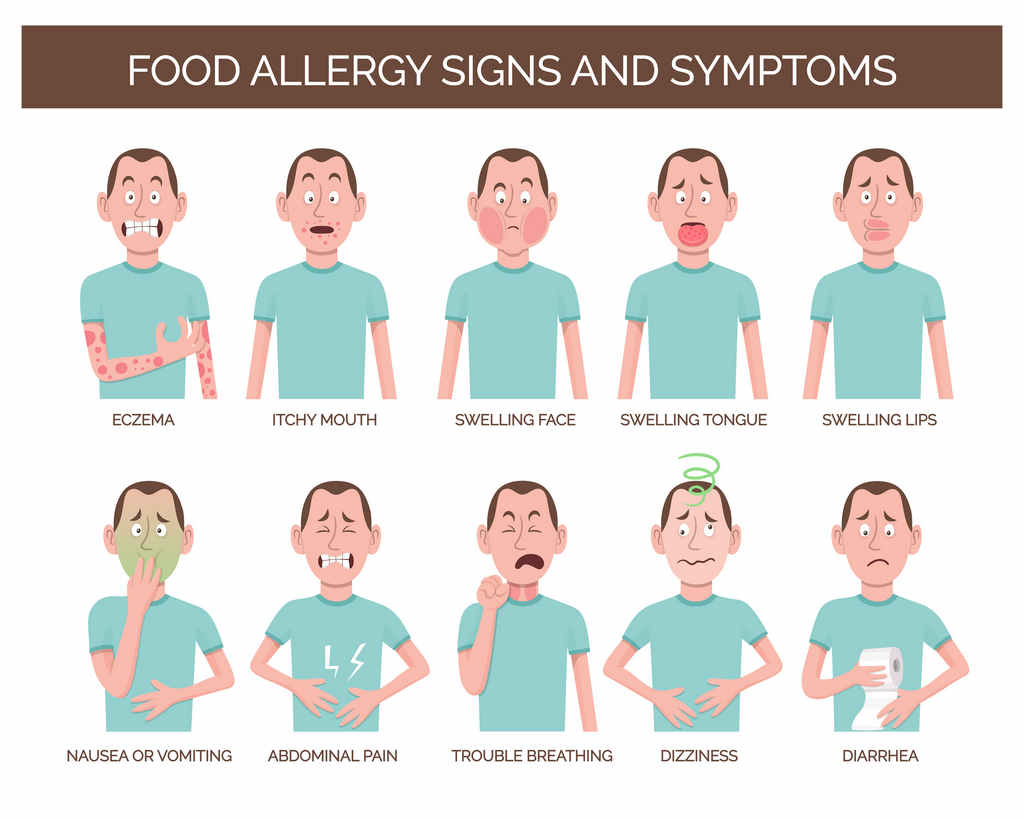
Food Allergies: Know the Symptoms
Symptoms of food allergies typically appear from within a few minutes to 2 hours after a person has eaten the food to which he or she is allergic. Allergic reactions can include:
- Hives
- Flushed skin or rash
- Tingling or itchy sensation in the mouth
- Face, tongue, or lip swelling
- Vomiting and/or diarrhea
- Abdominal cramps
- Coughing or wheezing
- Dizziness and/or lightheadedness
- Swelling of the throat and vocal cords
- Difficulty breathing
- Loss of consciousness
More Severe Food Allergy Symptoms
Initially mild symptoms that occur after ingesting a food allergen are not always a measure of mild severity. Following ingestion of a food allergen(s), a person with food allergies can experience a severe, life-threatening allergic reaction called anaphylaxis. This can lead to:
- constricted airways in the lungs
- severe lowering of blood pressure and shock (“anaphylactic shock”)
- suffocation by swelling of the throat
Each year in the U.S., it is estimated that anaphylaxis to food results in:
- 30,000 emergency room visits
- 2,000 hospitalizations
- 150 deaths
Prompt administration of Epinephrine by autoinjector (e.g., Epi-pen) during early symptoms of anaphylaxis may help prevent these serious consequences.
What Is Epinephrine?
It treats severe or life-threatening allergic reactions known as anaphylaxis. Anaphylaxis can occur after exposure to allergens such as:
- Food (like milk, eggs, shellfish and peanuts)
- Insect stings
- Latex
- Medications
How to Use an Epinephrine Injector*
- Grip the epinephrine pen firmly and remove safety cap.
- Swing and push the pen into the middle of the outer thigh at a 90° angle.
- Keep the pen pressed firmly against the thigh for 10 seconds.
- Remove the pen and massage the injection area.
*Always follow the manufacturer’s instructions for the specific injector you are using.
Food Allergy – Federal & General Resources
- AAAAI/ACAAI Practice Parameters
- Centers for Disease Control and Prevention
- Department of Agriculture
- Food Allergy Educational Materials – WIC Works Resource System
- Food Allergies and Intolerances – Nutrition.gov
- Department of Health and Human Services
- Food Allergies – Healthfinder
- European Academy of Allergy and Clinical Immunology: International Consensus (ICON) Papers
- FDA – Food Allergens
- FDA – Food Allergen Labeling & Consumer Protection Act – FAQs
- National Institutes of Health (NIH)
- Food Allergy – National Institute of Allergy and Infectious Diseases (NIAID)
- Addendum Guidelines for the Prevention of Peanut Allergy (2017)
- National Institute for Allergy & Infectious Diseases: Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary for Patients, Families and Caregivers (May 2011)
- National Institute of Allergy and Infectious Diseases, National Institutes of Health: Food Allergy
- National Library of Medicine
- Food Allergy – Medical Encyclopedia
- Food Allergy – MEDLINEplus